Links & Downloads
Throughout the history of Meals on Wheels, local providers have responded to the changing needs of the growing older adult population and the evolving landscape of demand, competition and funding. Today, rising costs, increasing need and growing waitlists underscore the urgency of strengthening and sustaining the Meals on Wheels network. Meals on Wheels America is committed to understanding the services, operations and experiences of local Meals on Wheels providers and how they are adapting to better serve the seniors in their communities, sustain services, serve more older adults and End the Wait™ for nutritious meals and moments of connection.
To support this work, Meals on Wheels America surveyed our membership of local Meals on Wheels providers to update and deepen our understanding of their services and experiences. This year’s report builds on the findings from the 2023 survey and will be followed by future updates to help uncover trends in waitlists, services provided and challenges faced over time, equipping Meals on Wheels America and the network with the needed insights to track progress and improve year over year.

Key Findings
This report details findings based on data from 628 providers that completed the online survey between June 21, 2024, and September 13, 2024. These findings are based on data from providers that offer direct home-delivered and/or congregate and/or grab-and-go meal services to their clients. Detailed findings are provided in the full report.
Services Provided
Nearly all (97%) provide home-delivered meals, and 72% provide congregate meals. A third (30%) provide grab-and-go meals, a service option that many began offering during the COVID-19 pandemic.
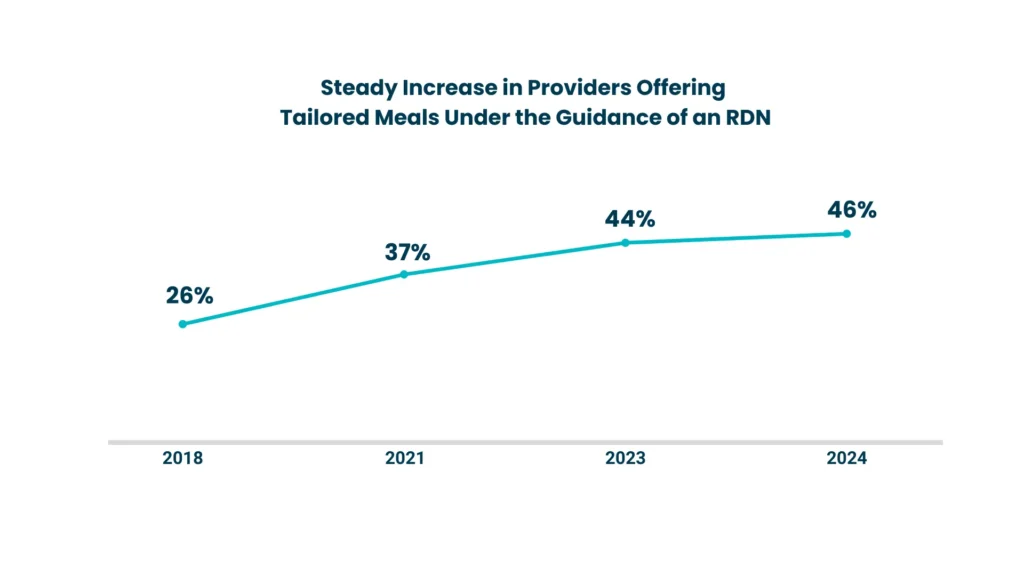
Providers see the need for tailored nutrition, and a growing number offer these services. Many providers identify medically tailored meals (82%), culturally tailored meals (41%) or both (29%) as the greatest need for tailored nutrition. At the time of the survey, 46% of providers that serve home-delivered meals offered medically tailored meals, a growing trend among providers.
Nearly all provide safety checks and social connection in some way, in addition to meals. Nearly all (96%) home-delivered meal programs train their drivers to keep an eye out for the senior’s well-being/general levels of health. Nearly 100% provide one or more social connection opportunities for at least some clients, such as conversations with willing clients during meal delivery (94%) or during congregate meals (92%), or other social connection opportunities, such as friendly visiting via phone/social calling (66%), socialization with other seniors beyond congregate meals (60%) and opportunities for clients to also be volunteers (e.g., mentoring, tutoring, social calling) (52%).
Providers vary in offering social connection opportunities specifically to clients identified as at risk for loneliness and social isolation. Of the 92% of providers that offer social connection opportunities beyond direct and purposeful conversation with clients at meals, only 19% prioritize social connection for clients identified as at risk for social isolation and/or loneliness. This suggests an opportunity for utilizing client assessments to ensure social connection services reach those most in need.
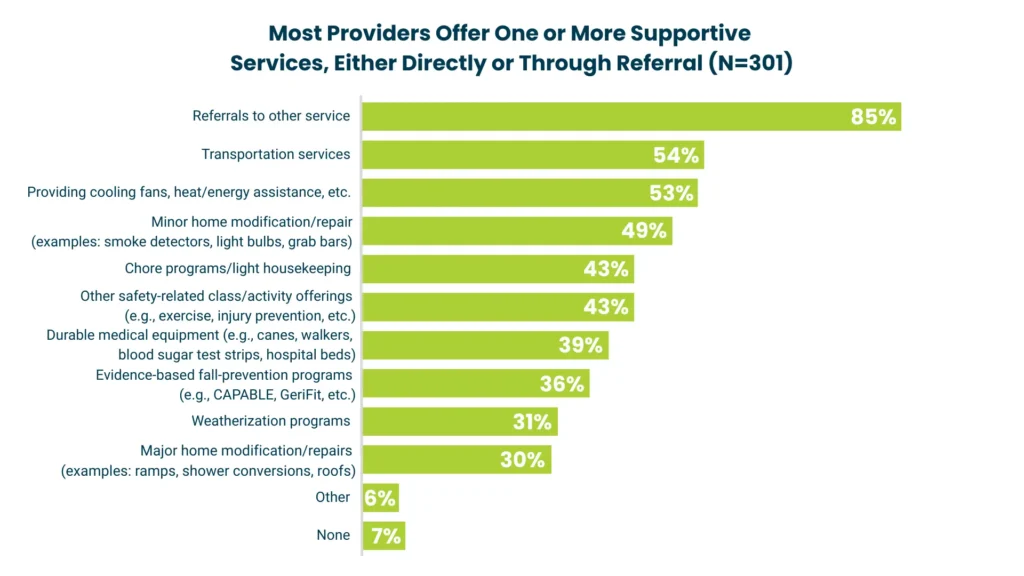
Many providers also offer other supportive services (93%), including referrals to other services (85%), transportation services (54%), cooling fans or heat/energy assistance (53%), and minor home modifications/repairs such as smoke detectors, light bulbs and grab bars (49%).
Funding Sources and Health Care Partnerships
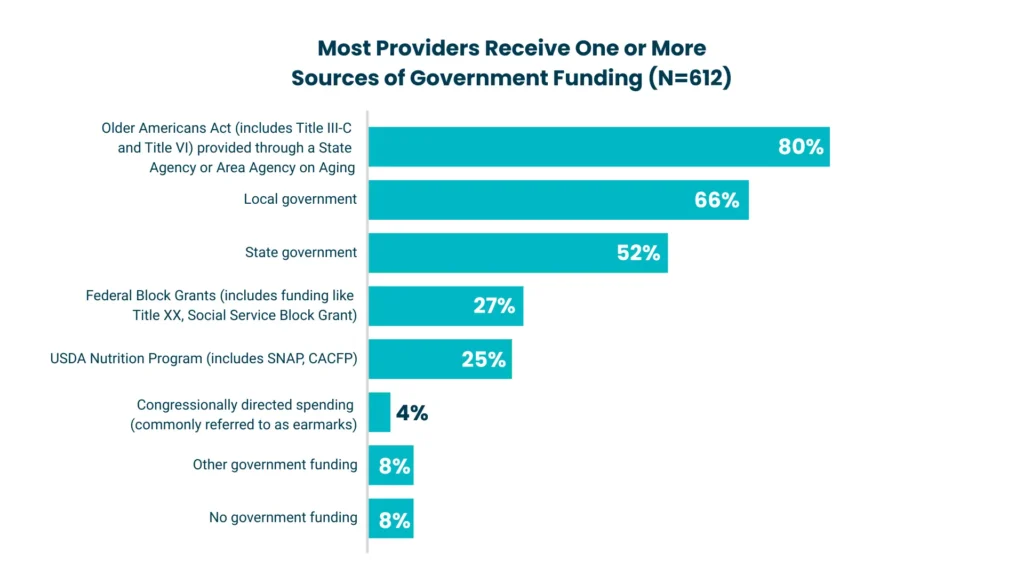
Providers receive funding from a variety of sources. Ninety-two percent of providers receive one or more sources of government funding for their senior nutrition budget, most frequently the Older Americans Act Nutrition Program (80%), local government (66%) or state government (52%). Nearly all (99%) receive one or more sources of private funding, such as client contributions or self-pay (93%), donor funding (personal or foundation, not including grants) (90%) or grants from non-government organizations (87%).
Nearly half of providers have some form of health care partnership. Forty-six percent of providers receive funds from or partner with a health-related organization (hospitals, health systems, community health centers, insurance companies, pharmaceutical companies). A third of providers that do not have a health care partnership plan to include this as a part of their growth strategy in the next two years.
Challenges and Accomplishments
Nearly all (98%) providers reported one or more challenges to serving meals to all seniors in their community who need them. Challenges that providers most frequently report include funding to pay for meals (71%), food prices (67%), recruiting and retaining enough volunteers (53%) and gas prices (42%). In open-ended comments, many providers described additional challenges related to increased demand for services and changing senior preferences.

Nearly all (99.8%) of home-delivery providers have taken actions due to funding challenges, up from 83% in our prior survey. Actions taken included using organizational funds to subsidize clients who are not funded and unable to pay (51%), tapping into their reserves to cover increased costs (47%), or adding seniors to waitlists (38%), up from 28% in our 2023 survey. In open-ended comments, some providers also mentioned service reductions or ending certain aspects of programs.
A third (33%) of providers report having a waitlist, with approximately 36,000 older adults waiting for meals across these organizations. The average wait time is nearly four months (115 days). An additional 12% of providers say they do not have a waitlist but may need one in the near future.

Despite these challenges, many providers are expanding services or facilities. In open-ended comments, providers reported expanding their services, such as adding new meal options, social connection opportunities, pet assistance programs and other innovations. Additionally, some reported expanding their facilities or equipment. Providers frequently mentioned that additional fundraising and partnerships (with pharmacies, schools, food pantries, farmers markets and health care organizations) helped them establish these new services and improved facilities.
Looking Ahead
These findings confirm what we already know: Meals on Wheels providers deliver more than a meal. Providers consistently offer needed nutrition, social connection and safety services, setting them apart from food delivery vendors that provide meals only.

However, the data also highlight a pressing need for greater resources to sustain and grow services. Across the nation, seniors are waiting months, or even years, for nutritious meals and moments of connection. As local providers work to End the Wait, rising costs, changing preferences of seniors and growing demand are straining organizations that are trying to do more with less.
Survey findings suggest several key areas that need to be strengthened for all providers to be able to deliver meals and other services that meet needs and preferences to all seniors in their communities who want and need them:
- Adequate, sustained and flexible public and private funding that keeps pace with increased demand and rising prices. This will need to include:
- Protecting and expanding federal, state and local government funding, especially through the Older Americans Act (OAA)
- Increasing private funding through philanthropy, corporate partnerships and public support
- Recruiting and retaining enough volunteers and staff
- Offering tailored meals
- Offering social connection services to participants identified as at risk of social isolation or loneliness
- Conducting outreach to raise awareness about available services and engage older adults to enroll in services
With federal funding failing to keep pace with need, a growing share of providers are relying on alternative private funding sources — reflecting both necessity and the increasing pressure to diversify revenue streams.
While these findings show the need for stable funding streams to sustain Meals on Wheels services and reduce the unmet need, they also remind us that funding to pay for the meals is only part of the solution. To provide the regular services that meet people’s needs and preferences, providers will also need adequate funding, tools and staffing for:
- Infrastructure, particularly recruiting and retaining enough volunteers and staff to serve current and new clients
- Providing meals tailored to meet the dietary needs of older adults’ medical conditions and align with local dietary practices and preferences
- Matching services to people’s assessed needs
- Outreach to assist older adults who can benefit from Meals on Wheels to enroll

Meals on Wheels providers are a vital, proven solution to support older adults with the nutrition, social connection and supportive services they need to safely age in place in their own homes. With enough funding and support, providers will be able to sustain services to current clients as costs rise, expand services to better meet clients’ needs and grow to serve all older adults in their community who are waiting for nutrition and social connection.
Download Full Report
In reproducing any excerpts of this report, please provide a credit that recognizes Meals on Wheels America, such as: Meals on Wheels America. (2025). State of the Meals on Wheels Network: 2025 Provider Benchmarking Report. https://www.mealsonwheelsamerica.org/research/state-of-the-meals-on-wheels-network-2025-provider-benchmarking-report

